[925] Experimental Ophthalmology
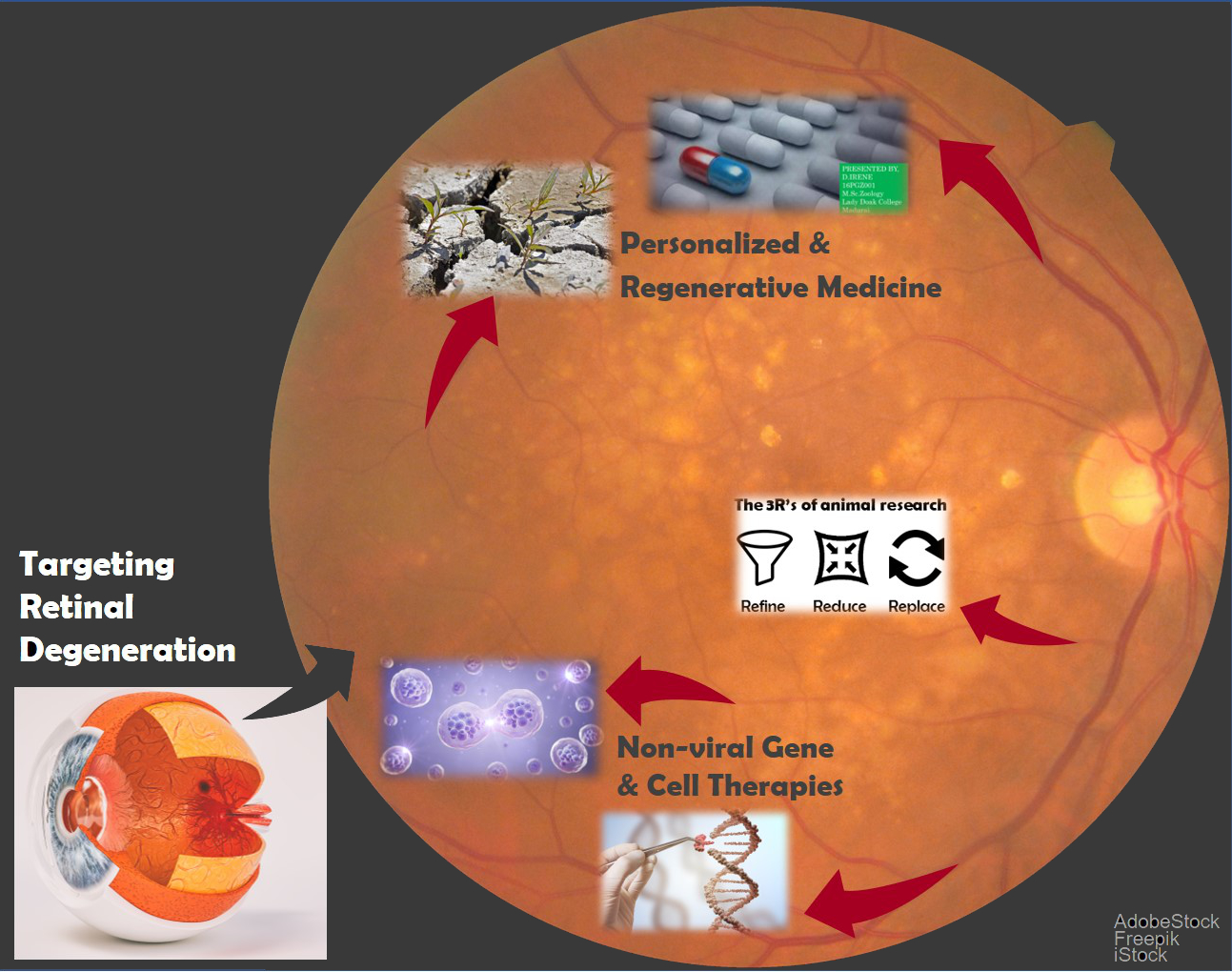
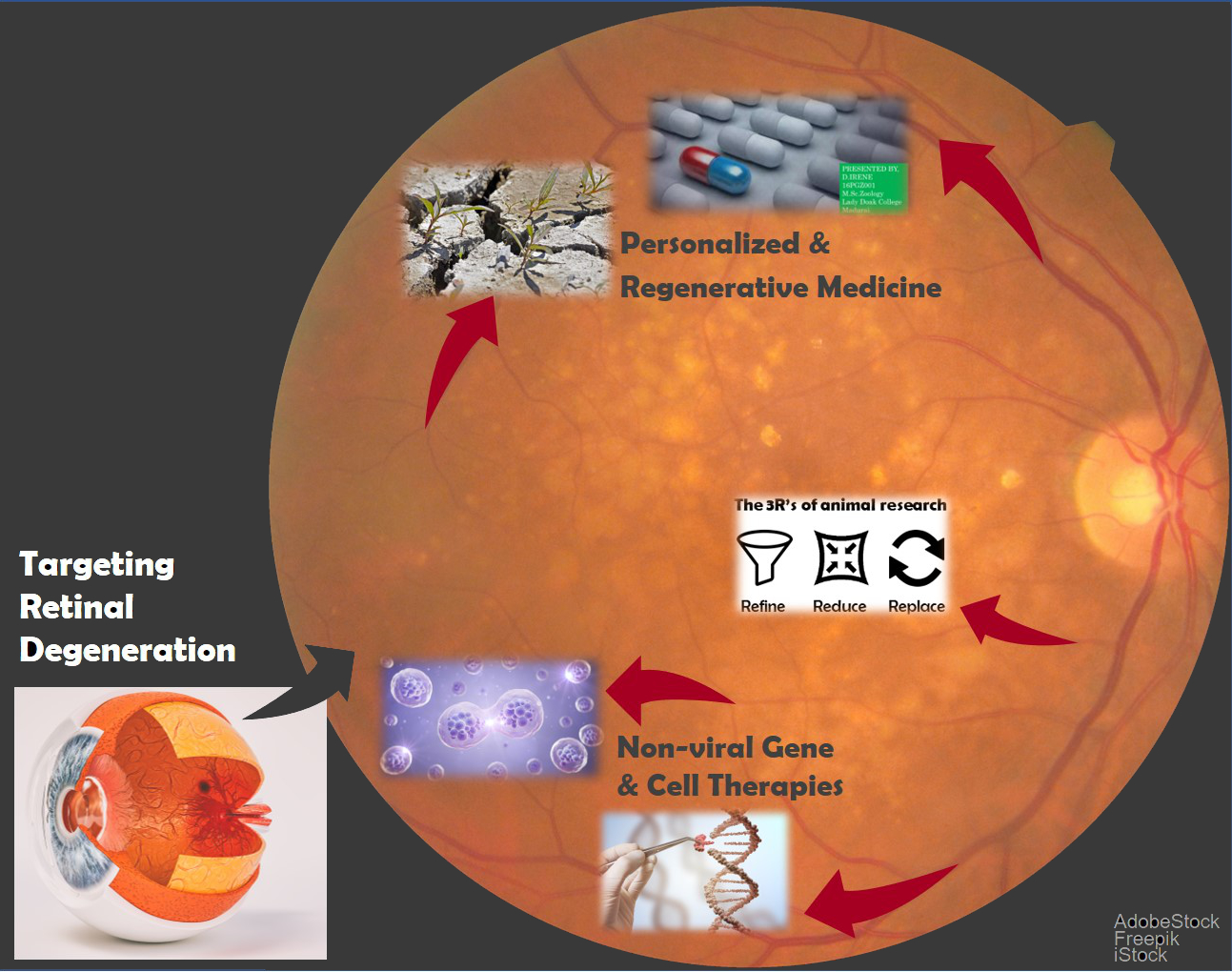
The group of experimental ophthalmology is a research and teaching center focused on optimizing the treatment of retinal diseases, such as age-related macular degeneration (AMD) and diabetic retinopathy. We are interested in regenerative and personalized medicine, and are developing cell-based, GMP-compliant (Good Manufacturing Practice) Advanced Therapy Medicinal Products (ATMP) to treat neurodegenerative diseases of the eye by developing regenerative gene therapeutic approaches, like the transplantation of genetically-modified and induced pluripotent stem cells. We are also working to reduce animal experimentation ("3R/4R": Refine, Reduce, Replace, [Responsibility]), in particular through retinal culture and cell culture free of animal products. Additionally, we are testing new biomaterials and innovative drug delivery systems.
Transposon-based gene cell therapy for the treatment of retinal neurodegeneration
We are happy to congratulate our student Mr. Mohit, who has been awarded the ARDITI prize 2023 in BIOLOGY, for his Master thesis entitled: "Up-scaling and humanization of retinal organotypic culture as a model for intraocular efficiency and toxicity analyses".
Currently, our research efforts involve the following projects:
In the TargetAMD project, (www.targetamd.eu) we developed a cell-based, personalized gene therapy treatment for neovascular (“wet”) AMD. The project was coordinated by Prof. G. Thumann and was funded by the European Union’s Seventh Framework Program for research, technological development and demonstration” (no. 305134), and carries on thanks to a grant financed by the ProVisu foundation. The therapy aims at suppressing vessel growth and at regenerating retinal architecture.
The project comprised various in vitro and in vivo development and validation steps during which we confirmed the efficiency and tolerability of the approach. After validation of the GMP-grade production of genetically modified iris pigment epithelial (IPE) cells, we received approval from the cantonal ethical commission for research (CCER) to perform a clinical phase Ib/IIa study. We are now awaiting approval from Swiss authorities, Swissmedic. The procedure comprises IPE cell isolation from an iris biopsy, genetic modification by the addition of the PEDF gene (Pigment Epithelium Derived Factor) using the non-viral Sleeping Beauty transposon system, and subretinal transplantation to the same patient, all within a single surgical session.
In contrast to wet AMD, in atrophic ("dry") AMD, the loss of retinal pigment epithelial (RPE) cells is not associated with new vessels proliferation, but probably results from inflammatory reactions and oxidative stress. Based on the non-viral gene therapy approach developed in TargetAMD, we aim to transplant genetically modified cells to continuously provide neuroprotective growth factors to the retina, to prevent further loss and degeneration of the RPE. In collaboration with Prof. L. Scapozza, UNIGE, we established in an in vivo model of dry AMD, and evaluate whether the transplantation of genetically-modified RPE cells supposed to express the genes coding for the proteins PEDF and GM-CSF (granulocyte macrophage-colony forming factor) prevents efficiently RPE cell death. We hypothesize that transplanted RPE cells will re-establish a neuroprotective retinal environment and inhibit the progression of the degeneration. Restoration of vision is analyzed by functional, behavioral, cellular and molecular methods. After in vitro proof-of-concept studies, we hope to demonstrate, in partnership with Prof. Z. Ivics, Paul-Ehrlich Institute, the safety of the treatment. This project is funded by the Swiss National Science Foundation (Funding: SNSF grants no. 160195 and no. 189341).
Stem cell-based, non-viral gene therapy to treat advanced dry AMD. The aformentioned approach is only suitable for patients at an early stage of the disease since damaged cells are not replaced. Stem cell therapies are currently under investigation to address this medical need. We hypothesize that cells transplanted into a damaged retina and a "toxic" environment cannot survive permanently. Therefore, we propose to combine the stem cell approach with our gene therapy to provide a permanent solution for patients with advanced dry AMD. We propose to genetically modify induced pluripotent stem (iPS) cells, differentiate them into RPE cells, and test in cell and retinal cultures the safety and efficacy of this new cell-based Gene Therapy Medicinal Product for the treatment of advanced dry AMD (Funding: Haas Foundation).
Retinal organotypic culture as valuable 3R compliant ex vivo model to test new drugs and therapies. We are culturing not only cells but the whole retina, and mimic pathogenic conditions (e.g. oxidative stress) to develop ex vivo models of retinal neurodegeneration, e.g., for dry AMD or diabetic retinopathy. Subsequently, the neuroprotective capacity of potentially therapeutic, protective proteins (PEDF and GM-CSF) overexpressed in transfected cells can be assessed by biochemical and immunohistological analyses. The retina culture system will be further enhanced in terms of culture duration, transferability and functionality. (Funding: SNSF grant no. 189341; Dr. Gaide AMD prize; Böringer Ingelheim).
Ocular in vivo electroporation to treat retinal neurodegeneration. We are developing a novel transfection (i.e. the introduction of a DNA sequence into the host genome) method using in vivo electroporation to target the RPE. Our goal is to simplify the treatment approach, and to increase the therapy’s safety. We are currently working with an eye model similar in size to human eyes. Further we plan to investigate an RPE-specific promotor to increase the safety profile of the approach. The project is carried out in collaboration with Prof. Z. Izsvák, Max-Delbrück Center for Molecular Medecin in the Helmholtz association. (Funding: Schmieder-Bohrisch foundation [terminated]; foundation; AURIS foundation [terminated]).
Subtype-specific molecular patterns in tear fluid of diabetic patients with and without retinopathy – predictive tool prototype. We aim to develop a diagnostic tool, which allows differentiating between patients, who are predisposed to severe proliferative diabetic retinopahty, from those likely to develop only a mild form or no retinopathy. To this goal, tear fluid samples will be collected and multiomic profiles determined in collaboration with Prof. Golubnitschaja, University of Bonn, DE, to identify biomarker patterns specific for distinct disease forms or phases. Tear fluid samples are easily and non-invasively collected, and their multiomic profiles reflect well the health status of a person, enabling fast, simple and personalized diagnosis and efficient and personalized management of diabetic patients. (Funding: LHW private foundation).
Xenofree ocular cell culture using human platelet lysate according to 3R/4R principles, to develop personalized therapy approaches. ATMPs (advanced therapy medicinal products), including regenerative, genetic and cellular therapies, have special requirements for production and quality control. One of the condition recommends the use of non-xenogenic reagents for cell culture to increase product safety; additionally, the use of FBS-alternatives is ethically favorable and responds to 3R/4R principles. We are developing a xeno-free cell culture system for ocular cells by using human platelet lysate from blood donation that satisfies both, the 3R principles of animal experimentation, and quality requirements of our cell products. The use of autologous platelet lysate to culture autologous cells will additionally improve patients’ security. (Funding: ARVO EyeFind Research grant).
Analysis of genetic factors in the pathogenesis of glaucoma and the analysis of therapeutic effects and mechanisms of action of KATP channel blockers. We found that the regulation of ATP-sensitive potassium (KATP) channels can lower the intra-ocular pressure (IOP) and affect aqueous dynamics. We hypothesized that a mutation in the KATP channel genes could be responsible for the increase in IOP in glaucoma. Indeed, in a pilot study we found three germline SNPs (Single-nucleotide polymorphisms) in the DNA of glaucoma patients, which might be involved in the increased IOP and retinal neurodegeneration. In the present project, we aim to collect saliva samples in a large cohort of glaucoma patients to analyze gene mutations involved in KATP channel opening and glaucoma pathogenesis. A study in rabbits investigates the benefit of KATP channel blockers in IOP lowering, aqueous humor outflow increase, and retinal ganglion cells’ protection. (Funding: Fonds Castier, HUG).
Other research interests include the development of quality controls for ATMPs during manufacturing using Raman spectroscopy; the analysis of the neuroprotective activity of scutellarin and the toxicity of decaline on the neural retina; the measure of the role of lysyl oxydase in diabetic retinopathy. In collaboration with Prof. D. Ghezzi, EPFL, we have established an in vivo model for the implantation of self-opening, intra-neural electrodes that allow stimulation of the optic nerve and the recording of its electrophysiological activity to restore vision through optic nerve prosthesis. The collaboration with Profs. T. Wolfensberger, M. Thiel, and Bignens is devoted to promote the development of personalized medicine by implementing the Swiss Ophthalmic Imaging Network (“SOIN”), a national secured system of ophthalmological data and diagnosis of patients. (Funding: Swiss Personalized Health Network).
Our clinical research comprises the transfer of therapeutic approaches developed in our laboratories into the clinic and clinical trials for new drugs and their mechanisms, as well as innovative surgical procedures (https://www.hug.ch/ophtalmologie/recherches-cliniques).
Published data are available on the repositories Yareta and Zenodo:
PUBLICATIONS OF THE GROUP