Thèmes et projets
Conflicts in the healthcare setting
Aims
To gather validity evidence for instruments that are used during the residency admissions process to assess the professionalism of applicants.
Persons involved :
|
UDREM-UNIGE
Nadia Bajwa Naïke Bochatay Katherine Blondon Pierre Chopard Stéphane Cullati Patricia Hudelson Fabienne Maître Virginie Muller-Juge Mathieu Nendaz Noëlle Junod-Perron Julia Sader Georges Savoldelli Nu Viet Vu
|
Collaborations Internationales
University of Washington Sara Kim
University of Szeged Marta Csabai Eva Csupor Agnes Kuna Judit Nora Pintér |
SUPPORTED BY :
University of Geneva
Résultats :
RESEARCH QUESTION 1 :
We sought to develop an understanding of how conflict is experienced by health care professionals working in diverse settings in an exploratory qualitative study with the aim of informing future conflict management training.
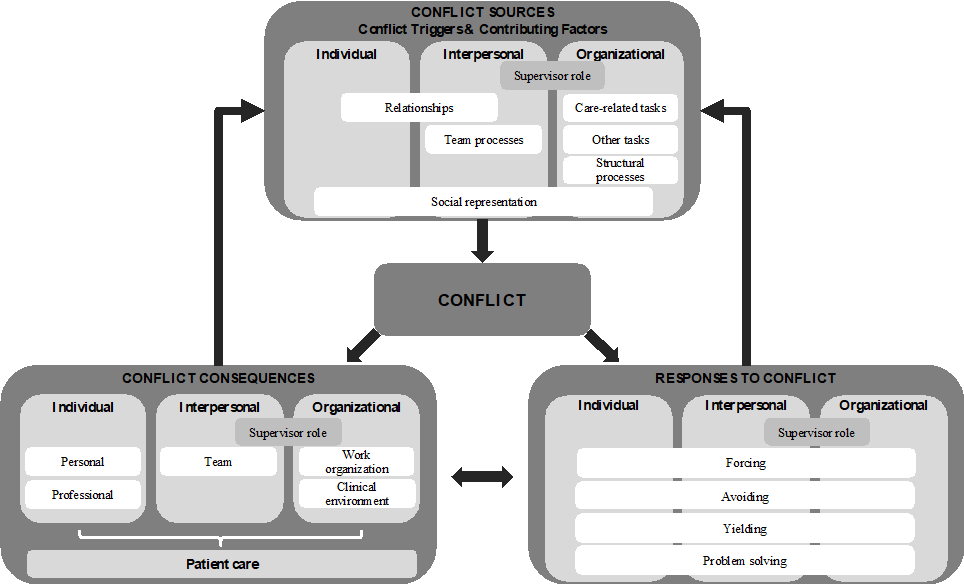
Through interviews with physicians, nurses, and certified nursingassistants from four departments in a teaching hospital, we have examined characteristics of professional conflict at the individual, the interpersonal, and the organizational levels.
Published in Academic Medicine
https://archive-ouverte.unige.ch/unige:99672
RESEARCH QUESTION 2 :
In this study, informed by social identity theory, we analysed semi-structured interviews on health care professionals’ experiences of conflicts to explore the interplay between group processes and conflicts, as well as the consequences of these conflicts on professionals.
This analysis of health care professionals’ experiences of conflicts using concepts from social identity revealed that hierarchy and power differentials were entangled with conflicts involving group processes. It also provided insights into dynamics within in-groups, as individuals struggled to be recognised as members of their in-groups and could become disillusioned with their professional ideals.
Published in Medical Education
https://archive-ouverte.unige.ch/unige:116626
RESEARCH QUESTION 3 :
In this study, we sought to compare and contrast characteristics of intra- versus interprofessional conflicts in the clinical setting, so as to inform our conceptual framework and future conflict management training programs.
Through our comparison of intra- and interprofessional conflicts, we have identified two main areas in which they differ. Intraprofessional conflicts were more likely to revolve around poor relationships and power differentials. Interprofessional conflicts, on the other hand, tended to be more closely related to patient care, as they arose from disagreements on patient-related tasks and affected the provision of care. Our results support the need to prepare learners to work in the clinical setting by providing them with training combining both intra- and interprofessional aspects to conflict management that reflect the reality of the clinical setting.
Published in the Journal of Interprofessional Care
https://archive-ouverte.unige.ch/unige:125542
RESEARCH QUESTION 4 :
The objective of this study was to explore health care professionals’ experiences of team conflicts and their perceptions of whether and how conflicts affected the multifaceted quality of patient care.
In a tertiary hospital, conflicts among health care professionals can potentially affect patient care. When team conflicts have consequences for patient care, they mostly influence timeliness, patient-centeredness, and efficiency. Quality managers of care hospitals should consider team conflicts as potential barriers to quality care. Quality management should consider preventive actions and support programs for management of conflicts.
Published in Mayo Clinic Proceedings: Innovations, Quality & Outcomes
https://archive-ouverte.unige.ch/unige:116821
RESEARCH QUESTION 5 :
This article examines how residents learn to manage uncertainty through two ethnographic case studies of academic medical centres in Switzerland and the United States (U.S.). It develops two models to show that supervision influenced how residents were trusted by supervisors, how they were awarded autonomy to practise independently, and how they grappled with uncertainty.
In shedding new light onto residents’ training for uncertainty in modern academic medical centres, this article describes two models for understanding how different attitudes towards uncertainty may develop.
In press
RESEARCH QUESTION 6 :
Using French and Raven’s social bases of power, we explored the role of power in conflicts between healthcare professionals in the USA, Switzerland, and Hungary. In doing so, we aimed to understand why power and conflict are often viewed negatively in healthcare in order to make recommendations to support a shift towards more constructive approaches.
By exploring the role of power in healthcare conflict across cultural contexts, we have shed light on key reasons why power and conflicts are viewed negatively. These reasons include perceived misuse of individuals’ position, unequal statuses between professions and specialties, and difficulties associated with shifts and work hours. Another reason related to the frequent presence of an audience when delivering healthcare work, such as supervisors, co-workers, patients, and families. Our findings suggest that fostering more positive approaches towards power and conflict could be achieved by using social bases of power such as referent power and by addressing conflicts at the backstage in a more private manner.
In press
