Introduction
Definition
Obesity is defined as an unhealthy amount of body fat (45) or, in other words, an excess of fat (triglycerides) storage in the adipose tissue (19).
The most appropriate tool to quantify the degree of obesity is the Body Mass Index (BMI) or Quetelet Index. This index is calculated by dividing one's weight (in kg) by the square of one's height.
BMI = mass (kg) / height² (square m)
The reference values of BMI are identical for both sexes (table 1):
Prevalence and incidence
Obesity increased dramatically its prevalence the last 20 yeas (91, 72, 36). Obesity became a big health problem for the modern, developed countries. Great Britain obesity's prevalence doubled between 1980 and 1991 to reach nearly 20% of the population. Some other country averages are: USA - which detains the record - 25%; France, Sweden and Holland 7-10%.
Morbidity
Morbidity is an important feature when we talk about obesity. If there is some debate if there is a health benefit of being thinner among the individuals whose BMI is less than 25, there is no doubt that a BMI over 25 confers increased health risk. Overweight and obesity have been associated with an increasing risk of a large number of disorders including, but not limited to the following :
-
Dyslipidemias (25,26) characterised by :
- high total cholesterol (> 2.40g/l) - more than 25% prevalence for BMI bigger than 30
- high LDL (low density lipoproteins cholesterol) >1.6 g/l which is a risk factor for cardiovascular disease (CVD)
- low HDL ( high density lipoproteins cholesterol) <0.450mg/l, which is a protection factor against the CVD
- high triglycerides (>2.5g/l)
- Non-Insulin Dependent Diabetes Mellitus (NIDDM). It has been shown that excessive adipose tissue is associated with increased insulin resistance.
- Hypertension
- Coronary heart disease
- Osteoarthritis in the weight bearing joints
-
Cancers :
- breast cancers in postmenopausal women which might be due to the estrogenic secretion of the adipose tissue
- colon cancer
- endometrial cancer
- Sleep apnoea and respiratory disorders are present in up to 24% of overweighted man and 9% of overweighted women (Allison DB '00)
Factors influencing the weight gain
Both increasing prevalence and morbidity of obesity have multiple causes. Among the most important factors in the development and persistence of obesity we remind the following:
- age - maximal prevalence is found between age 60 and 70 years old.
- sex - female > male (91)
- heredity -genetic predisposition that determines a bigger susceptibility of a person to gain weight into a given environmental context (86). The impact of heredity is estimated at 25-40% for obesity in general and 50% for abdominal obesity (13)
- geographic region -the Eastern and the Northern part of Europe are prone to an increase prevalence of obesity (72,91)
- social level - the maximal prevalence is in the poor communities of developed countries (82,83)
-
life style
- industrialisation and urbanisation have reduced considerably the energy expenditure of the individuals (34, 45) and physical exercise became optional (46). There is a direct, positive correlation between obesity and the lack of physical activity. The time spend per day watching TV is proportional with the degree of obesity (2, 27, 41, 92).
- the evolution in food intake is characterised by the decrease in complex sugars intake - as fibbers from fresh fruits and vegetables - and by the increase in lipid intake, mostly of animal origin. The vast majority of the industrially prepared food has a high caloric density, much higher than the traditional meals.
Physical exercise limits the decrease in energy expenditure (EE) at rest, that appear with ageing and explain the weight gain in elder persons (46, 90).
Psychological factors
The role of psychological factors in inducing obesity is controversial. Historically, prevailing opinions on the relationship between obesity and the psychological profile have varied greatly. In the 1960s and prior, the belief was hat obesity was, in part, caused by certain psychological abnormalities. At that point, most of the studies were based on limited samples of obese people seeking treatment (32). A study published by Stunkart and Mendelson (1967), caused the pendulum to swing in the other direction. By examining a less specific, wider sample of obese persons, it was concluded that the previous opinion might have been incorrect. The authors found that in a large, non-clinical community-based sample, there was no meaningful association between obesity and gross pathology. From the influence of Stunkard and those who followed in the 1970s and 1980s, it was generally thought that either there was no real correlation between obesity and psychological adjustment, the attendant social stigma caused psychological maladjustment and not the reverse. In the 1990s, a greater complexity is being acknowledged (36). There is accepted that there may be a complex interrelationship between psychological profile and obesity, but causal direction is unclear.
Binge eating disorder (BED) - eating very fast a huge amount of food in response to psychological stimuli instead of hunger, followed by a feeling of culpability and poor self esteem - is viewed as the major psychological disorder of obese persons. It occurs in about 40% of the obese persons (80). Among those subjects BED is associated with increased adiposity and frequent, significant weight fluctuations (81, 29, 15). This explains the difficulty of maintaining the low weight levels achieved after treatment especially in BED patients.
Compared with non-BED obese subjects, BED obese patients have lower self-esteem, poorer sense of personal effectiveness, more disturbed self-attitudes and higher levels of depression, anxiety and personality disturbances (89, 94).
Even if we don't know the sense of the causal relationship between obesity and psychological disorders, we can notice that morbidly obese persons have a real psychological and somatic sufferance, which lowers considerably their quality of life.
The psychological aspect is marked by different degrees of anxiety and depression. Both of them are significantly improved by the stable weight loss.
Treatment
It have been demonstrated that even a small decrease in body weight, (i.e. of 5-10%), is associated with clinically important improvements in cholesterol levels, blood pressure, glycaemia and other health indices (40). These benefits persist if the weight loss is maintained (95). Those findings as well as the huge increasing in prevalence of obesity and its complications have justified substantial efforts in finding effective methods for loosing weight and maintaining stable low weight.
a) Food restriction diets
The food restriction was, historically, the first approach in treating obesity but, unfortunately, with poor long-term results. Diet, as unique treatment, induces or aggravates the eating disorders. The complications of dieting are: gaining more weight (by the means of reducing the metabolism at rest), increasing morbidity of obesity, inducing weight cycling and diminishing the psychological status of the patient. As an example, all the studies that followed patients for 5 years or more after a successful food restriction diet - which means loosing at least 10% of their initial body weight - showed that almost all the patients have reached or exceeded their initial body weight after 5 years (54, 96, 19 etc.). This is why, at present, the food restriction alone it is no longer recommended as treatment of obesity.
b) Cognitive- behavioural approach
Association of cognitive-behavioural approach to the food restriction or to a regular, healthy, diet was thought to be the solution in treating obesity. Unfortunately this was not the case. Excepting the improvement in the eating behaviour and anxio-depressive disorders, the weight loss was disappointing (69).
c) Drug treatment
Drugs alone or in association with previous types or therapies gave place to big expectations. There are a few classes of drugs used in the treatment of obesity :
- anorexic agents divided in two commonly used families: noradrenergics and serotoninergics. A third family, the fenfluramins, induce dependence, have a poor efficiency and severe adverse reactions. Their use is limited at max 3 months.
- drugs that diminish the energetic intake - as Orlistat that is a selective and powerful inhibitor of gastric and pancreatic lipase inducing steatorrhoea . At the moment orlistat is the most reliable drug in the treatment of obesity.
- drugs that increase the energy expenditure - thermogenetic agents are not effective in humans. Ephedrine and xantines have a significant effect on loosing weight, but the benefit and risk balance is not sufficiently evaluated.
Unfortunately none of those substances can give a solution to the big problem that is obesity either because of the induced risks, or of their inefficacy.
d) Surgical treatment of obesity, so-called - bariatric surgery
Because current treatments, as we have seen, are usually ineffective in patients with morbid obesity, surgical methods (especially Roux-en-Y gastric by-pass) have been assessed. The success rate in achieving and maintaining long term weight loss is 80% or greater, significantly higher than with any other treatment (16).
Results of bariatric surgery
What do we expect from surgical methods of loosing weight - called bariatric surgery - in terms of results? Patients lose after the gastric bypass, around 50-60% of their excess body weight in the first year and they can generally maintain the weight loss at 5 years with only a modest regain of 5-7 kg (18, 64, 8). These long term results makes the bariatric surgery the only way of loosing weight and maintaining weight lost for the morbidly obese persons.
Classification of the bariatric procedures :
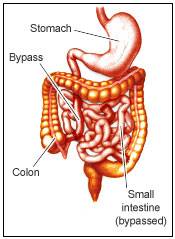
- Gastric Bypass (GBP), the most used is the Roux en Y GBP technique (see description below)
- Horizontal Gastroplasty
- Vertical Gastroplasty
- Gastric Banding
- Biliopancreatic Diversion
- Jejunoileal Bypass
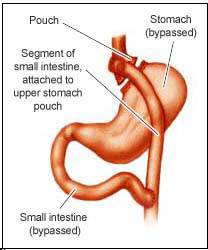
1. Gastric Bypass (GBP)
The gastric bypass (GBP) is considered by many to be the gold standard of the bariatric surgery.
Historical data on GBP
The GBP has been practised on humans since 1967 and has undergone many modifications ever since. The prototype was Billroth II gastric operation but without removal of the distal stomach.
GBP description
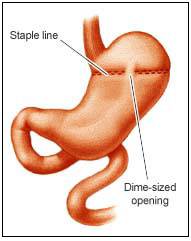
The GBP consists in creating a small pouch of 30cc from the upper stomach by stapling and therefore, separating the stomach in two separate compartments. The 30cc stomach pouch is drained into an intestinal loop (Roux en Y loop, most frequently) made by the small bowel (fig. 1). To bring the bile and the pancreatic secretion for the normal digestion, another surgical anastomosis is practiced between two loops of the small bowel at various distances from the ileo-caecal valvulae, for ex: 50-60cm for distal Roux en Y GBP.
The mechanism of GBP functioning
GBP causes weight loss - by diminishing caloric intake - through multiple mechanisms :
- decreased capacity of the stomach that produces rapid sensation of satiety with even minimal food intake
- restricted rate of emptying the pouch
- prohibiting, by the apparition of the dumping syndrome, the ingestion of certain hyper osmolar foods (generally the sweet food containing sugar, glucose, etc., which are generally calories-dense foods)
2. 3. 4. Horizontal Gastroplasty, Vertical Gastroplasty and Gastric Banding
Those are techniques by which the stomach is divided in two pouches that communicate one to another (fig. 2 and 3). The only mechanism of loosing weight, in this case, is the mechanical restriction of the quantity of food intake. That's why the long-term results are poorer than with the GBP.
Inconvenients of the gastroplasties (gastric stapeling)
- the enlargement of the gastro-gastric stoma (fig. 2)
Inconvenients of the gastric binding (fig. 3)
- the slip of the band
- the difficulty of establishing the limit between the tightness (with vomiting) and the loseness (with weight gain)
 |
 |
 |
5. Biliopancreatic diversion (BPD)
Developed by Scopinaro in Genoa, has some similarities to the distal Roux en Y distal GBP (fig. 6), but a subtotal gastrectomy is performed and a gastric pouch of 200cc to 400cc is left. There is a wide stoma between the gastric poach and the gut to permit adequate meals and avoid the major sequelae, hypoalbuminemia, which occurred in about 10% of patients (Scopinaro N, Probl. Gen. Surg. 9:298).
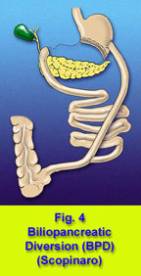
Inconvenients of BPD
- fatty, soft stools - 2 or 3 per day
- calcium and fat-soluble vitamin malabsorbtion that require adequate supplementation
- it is a procedure of a certain magnitude
6. Jejunoileal Bypass (JI)
Performed at large scale in the '60s-'70s JI (fig. 5) has been abandoned because of the high incidence of the complications.
Complications of JI
- anaerobic proliferation on the blind loop with secondary abdominal distension
- absorption of bacterial products led to circulating immune complexes with polyarthralgies that usually responded to antibiotics (24)
- calcium oxalate nephropathy caused by the absorption of calcium oxalate and favourised by dehydration caused by diarrhoea
- diarrhoea
- hepatic insufficiency
Considering all previous data and the complex profile of the morbidly obese individual, those patients should be selected and clinically followed by a multidisciplinary team. This team consists in: physicians with special interest in obesity, dieteticians, psychologists or psychiatrists interested in behaviour modification and eating disorders and a surgeon with experience in bariatric procedures.
Hypothesis
We clinically observed that the most obese of our patients have more difficulties to correct their BMI after the GBP. Our hypothesis is that those patients might be psychologically different from the less obese individuals of our group (BMI < 44 kg/m2) and this difference might play a role in loosing weight after the GBP.
The purpose of our study is to determine the relationships or even the correlations, between the pre-surgery psychological profile of morbidly obese subjects and the post-surgery outcome, in terms of loosing weight.
Question
What it would be interesting to know, but there is no available coherent data, is :
- Who will be the best subject for the bariatric surgery? In other words: is it possible, using the pre-surgery data only, to predict who will lose a satisfactory amount of weight without any psychological complications (suicide, alcoholism, worsen BED etc.)?
- Is there a method to improve the weight loss after the GBP? If yes, which subgroup of patients would benefit the most?