A pair of genes could predict cancer progression
A UNIGE team has identified two key genes whose expression influences cancer progression.
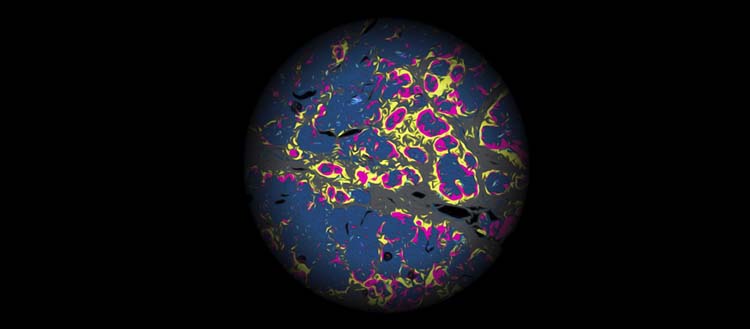
© Mikaël Pittet. A view of the tumor microenvironment. Magenta: macrophages expressing CXCL9. Pale blue: macrophages expressing SPP1. Dark blue and yellow: tumor cells. Grey: stroma.
Tissues, blood vessels, cells: tumours develop in a complex ecosystem known as the tumour microenvironment. While it is established that this environment differs from one patient to another and that it can have a positive or negative influence on the progress of the disease, the rules that govern tumour microenvironments are still poorly understood. A team from the University of Geneva (UNIGE) has succeeded in deciphering one of them by identifying a pair of genes whose expression can accelerate, or slow down, the progression of cancer. These promising results are published in the journal Science.
The ecosystem in which a tumour develops is known as the tumour microenvironment. Made up of blood vessels, immune cells and other apparently normal cells, it constantly interacts with tumour cells. These components, which differ from patient to patient, have a crucial influence on the course of the disease: they can speed up or slow down its progression. However, the mechanisms governing their variations and interactions are still poorly understood.
"The very different manifestations of cancer from one patient to another are often a major difficulty in research. Here, on the contrary, we have been able to take advantage of these variations to highlight the rules that govern the course of the disease," explains Mikaël Pittet, full professor at the UNIGE Faculty of Medicine, holder of the ISREC Chair in Immuno-Oncology, director of the Centre for Translational Research in Onco-Haematology and a member of the Lausanne Branch of the Ludwig Institute for Cancer Research.
Two key genes
Until now, most studies have involved populations of cells from tumour ecosystems from different patients, grouped together and observed indistinctly. This method makes it possible to classify tumour microenvironments on the basis of general criteria, but not to analyse their variations from one individual to another. To remedy this, the team led by Mikaël Pittet examined separately 52 head and neck tumours taken from the same number of patients. They were thus able to compare them and identify a key parameter governing tumours: the expression of the CXCL9 and SPP1 genes by immune cells known as macrophages.
"Within tumour microenvironments, these two genes are expressed antagonistically by this particular type of cell," explain Ruben Bill, postdoctoral researcher, and Pratyaksha Wirapati, bioinformatician, both co-first authors of the study and members of Mikaël Pittet’s group, "We found that patients with high expression of CXCL9 relative to SPP1 in macrophages had better clinical outcomes than those with the opposite proportion".
Macrophages expressing more of the first gene are involved in attacks on cancer cells, while those expressing more of the second participate in their growth. Tumour macrophages are able to engage in one or other of these programmes, depending on the CXCL9 and SPP1 genes they express. This is known as macrophage "polarity".
Wider implications
To their surprise, the scientists discovered that this polarity is linked to all the components of the tumour ecosystem. Thus, when the ratio of CXCL9 to SPP1 is high in macrophages, the activities of other cells also take on an anti-tumour orientation, and vice versa when this ratio is reversed.
"The single observation of the ratio of this pair of genes in macrophages therefore makes it possible to deduce the overall activity of the cells that make up the tumour microenvironment. In other words, tumour microenvironments appear to be governed by coherent and relatively simple internal rules. This study has enabled us to describe one of them," enthuses Mikaël Pittet.
For the researchers, the next steps will be to determine how to interfere therapeutically with these networks, and how best to adapt treatments according to the tumour characteristics of each patient.
3 Aug 2023