Cystic fibrosis: why infections persist despite therapy
A UNIGE team discovered that treatment for cystic fibrosis does not eliminate the docking stations of bacteria responsible for respiratory infections.
Adobe Stock - UNIGE. Cystic fibrosis is a genetic and hereditary disease affecting specific cells - epithelial cells - lining certain organs, including the respiratory epithelium in our lungs (inset).
Cystic fibrosis is a genetic disease that causes serious and sometimes fatal respiratory and digestive disorders. A new treatment, available since 2020, improves lung function and quality of life. However, it does not always eradicate the bacteria responsible for respiratory infections. By studying 3D models of human lung cells, scientists at the University of Geneva (UNIGE) discovered that this drug does not prevent the development on the surface of the respiratory tract of ''docking stations'' to which bacteria attach themselves to infect the body. These docking stations result from a disruption in the signals involved in cell development in the respiratory system. By combining the current treatment with other molecules, it may be possible to restore cell balance and thus better prevent bacterial infections. These results are published in the American Journal of Respiratory Cell and Molecular Biology.
Cystic fibrosis is the most common genetic disease. Each year, it affects one in every 3,300 newborns in Switzerland. Mutations in the gene responsible for the CFTR protein cause the secretion of excessively thick mucus, which obstructs the airways. Although a triple therapy, available in Switzerland since 2020, has improved the quality of life of people with cystic fibrosis, it is not suitable for all those affected and does not always prove effective.
‘‘A significant proportion of people who take this treatment still suffer from residual inflammation and persistent respiratory infections. Understanding the reasons for this is essential if we are to improve patient care,’’ explains Marc Chanson, full professor in the Department of Cell Physiology and Metabolism in the UNIGE Faculty of Medicine and member of the Geneva Inflammation Research Centre, who led this research.
An imbalance in cell signals
In previous studies, Marc Chanson’s team had discovered that respiratory cells affected by cystic fibrosis build on their surface docking stations that enable bacteria to firmly anchor to the lungs. ‘‘We therefore wanted to find out whether triple therapy had an effect on this mechanism, which is so predisposing to bacterial infection,’’ explains Mehdi Badaoui, research and teaching fellow in the Department of Cell Physiology and Metabolism in the UNIGE Faculty of Medicine and last author of the study.
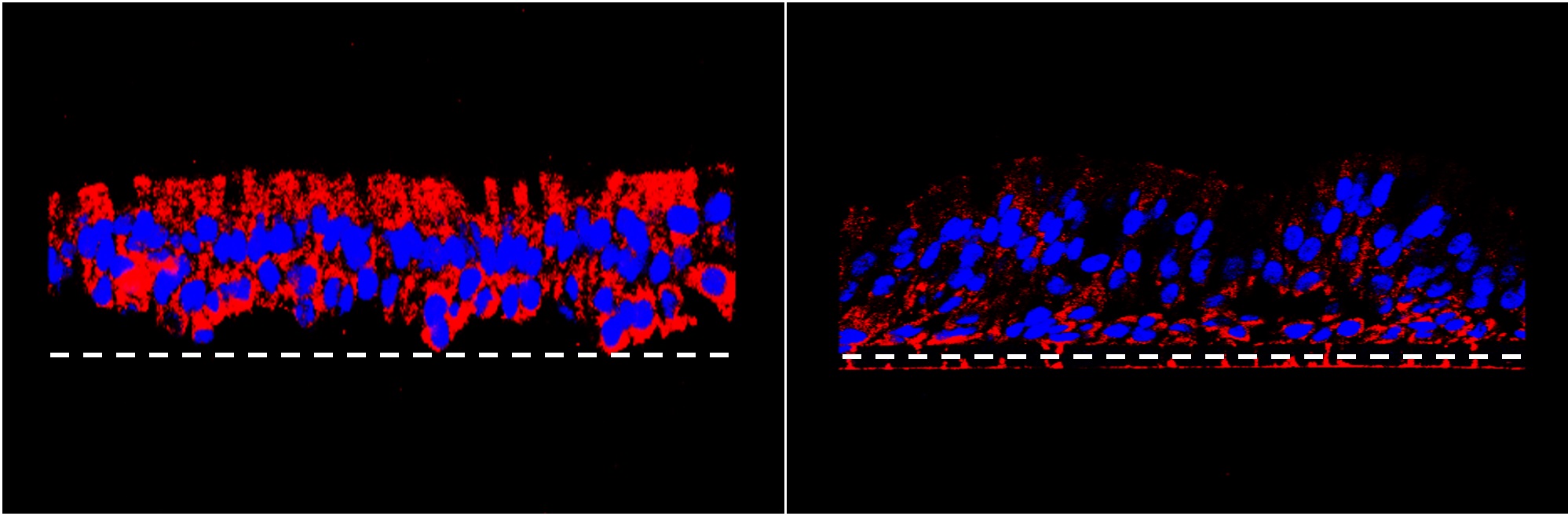
The anchor points present on the surface of the airways in cystic fibrosis (left image, in red) decrease when the balance between the two cell signalling pathways is restored (right image).
By comparing 3D models of human lung cells — healthy cells as well as cells with cystic fibrosis — the scientists demonstrated that the triple therapy currently used does not prevent the formation of these docking stations. Indeed, gene expression in healthy cells, compared with cystic fibrosis cells, shows an imbalance between two cell signalling pathways: the TGF-β pathway is hyperactivated, while the Wnt pathway is inhibited. Cell signalling pathways underpin the development of all multi-cellular organisms, including humans. Without them, cells are unable to develop and function properly.
By revealing a disruption in these signalling pathways, the research team shed light on a key mechanism: diseased cells do not receive appropriate signals and react by creating docking stations that are harmful to them. By restoring the balance between these two cell signalling pathways, the scientists were able to significantly reduce the development of these structures. ‘‘If we manage to identify a pharmaceutical compound capable of restoring this balance in patients, we could then combine it with the current triple therapy to increase its efficacy and limit bacterial infections, while reducing its side effects,’’ concludes Marc Chanson.
4 Apr 2024