Poor wiring in the centre of the brain leads to psychosis
Psychosis is linked to abnormalities in brain development. A team from the Synapsy National Centre of Competences in Research has demonstrated that the regions of the brain involved in processing memory, imagination and emotions in people with psychosis have poor connectivity from childhood.
The main characteristics of psychosis are loss of contact with reality, sudden delusions and irrational thoughts. The condition – which may be a symptom of a serious mental illness, such as schizophrenia – appears in late adolescence, with around 3% of the population experiencing at least one psychotic episode. Neuroscientists think that psychosis is caused by subtle neurodevelopmental abnormalities during childhood and adolescence. It follows that the discovery of brain structures and neurobiological mechanisms linked to the early stages of psychotic disorders is arousing considerable interest, since it could lead to new treatments.
Genetics: in the right place at the right time
The research team led by Stéphan Eliez, a professor in the Faculty of Medicine at the University of Geneva (UNIGE) and a member of Synapsy – the Swiss National Centre of Competences in Research into Mental Illness – is particularly interested in people suffering from 22q11 deletion syndrome (22q11DS). This is a congenital genetic defect in which part of chromosome 22 is missing: individuals with this deletion have a 30% to 40% risk of developing psychotic symptoms. “This high percentage means we can study the neurodevelopmental bases of psychosis during childhood, with a greater chance that, once they are adolescent, they develop psychotic symptoms”, begins Farnaz Delavari, a doctoral student and clinician at UNIGE and the study’s first author. In fact, only one person in a 100 without the deletion develops a psychosis. In addition, there are laboratory mice that are carriers of the same genetic deletion, which facilitates the work of researchers before they transfer and apply their findings to human neuroscience.
In a study published in the journal Biological Psychiatry, Professor Eliez’s team, working closely with an EPFL laboratory specialising in neuroimaging, followed a cohort of 22q11DS patients aged 6 to 35 years. As Delavari explains, the patients received a functional MRI neuroimaging scan every three years: “This meant we could observe the different individual trajectories, both in terms of cerebral functions and the structure of the brain as well as psychotic development”.
Deep and early dysconnectivity
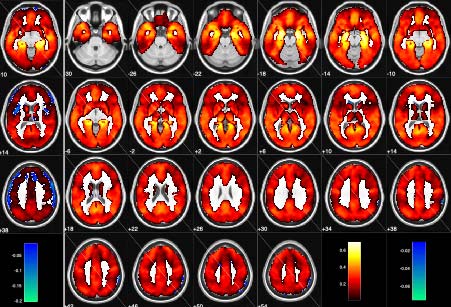
The Synapsy researchers focused in particular on the development of the hippocampus, a deep structure that processes information from other parts of the brain and that plays a central role in memory and spatial navigation. Structural and functional alterations in the hippocampus are well known not just in psychotic patients but also in 22q11DS mice. The latter are thought to have problems during adolescence synchronising the hippocampus with the prefrontal cortex, a region of the brain where various so-called superior cognitive functions are situated, including reasoning, working memory, language and executive functions. Delavari continues: “We have developed a new methodological approach so we can detect the maturation of the connectivity of the hippocampus linked to the appearance of psychotic symptoms”.
The study reveals that the hippocampus in individuals affected by 22q11 deletion fails to develop a mature form of connectivity with the prefrontal cortex. Furthermore, their hippocampus remains immature, or hyperconnected to dopaminergic neuronal fibres, as is the case in children. These dopaminergic pathways have numerous functions, such as learning, reward and motivation, and are known to play a part in various mental illnesses, including schizophrenia.
A limited window of opportunity
“Our observations,” resumes Professor Eliez, “suggest that the cortex doesn’t control the hippocampus enough during development, which results in neuronal hyperactivity in the hippocampus, leading to its atrophy”. This defect in brain development plays a crucial role in psychosis, according to the researcher, via an abnormal processing of memory, imagination and emotions in the hippocampus. “The hippocampus’s connectivity could be a target for new early intervention strategies, prior to adolescence, designed to prevent the onset of psychosis, especially since we already know of drugs that can preserve the development of the hippocampus.”
By Yann Bernardinelli, Press Officer NCCR-Synapsy
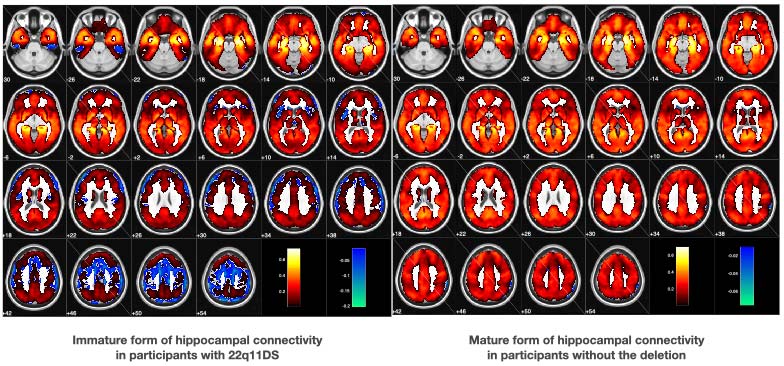
In young adults with the 22q11 deletion (left), hippocampal connectivity is not as mature as in people without the deletion (right). ©UNIGE/Eliez
2 Mar 2021