Opening the back-door for natural antibiotics
The discovery of antibiotics – natural chemotherapeutics produced by other microbes that can be used to kill or inhibit the growth of bacteria - at the beginning of the 20th century was perhaps the greatest achievement of human medicine. Unfortunately, the overuse of antibiotics facilitated the emergence of antibiotic-resistant bacterial strains that escape antibiotic therapy, an occurrence that is particularly frequent among Gram-negative (diderm) bacterial strains. The World Health Organization (WHO) estimates that death of over 5 million people annually is linked to (opportunistic) bacterial infections that no longer respond to antibiotic treatment, and this number is likely to increase as their prevalence increases commensurate with the population with weakened immune systems such as newborns, the elderly, transplant and cancer patients. Thus, new strategies are needed to combat bacterial infections. A team of researchers in the MIMOL department now reports a previously unknown mechanism in The Embo Journal describing how excessive zinc ions (known as zinc stress) open an entry gate for certain large antibiotics that are normally unable to permeate Gream-negative bacteria.
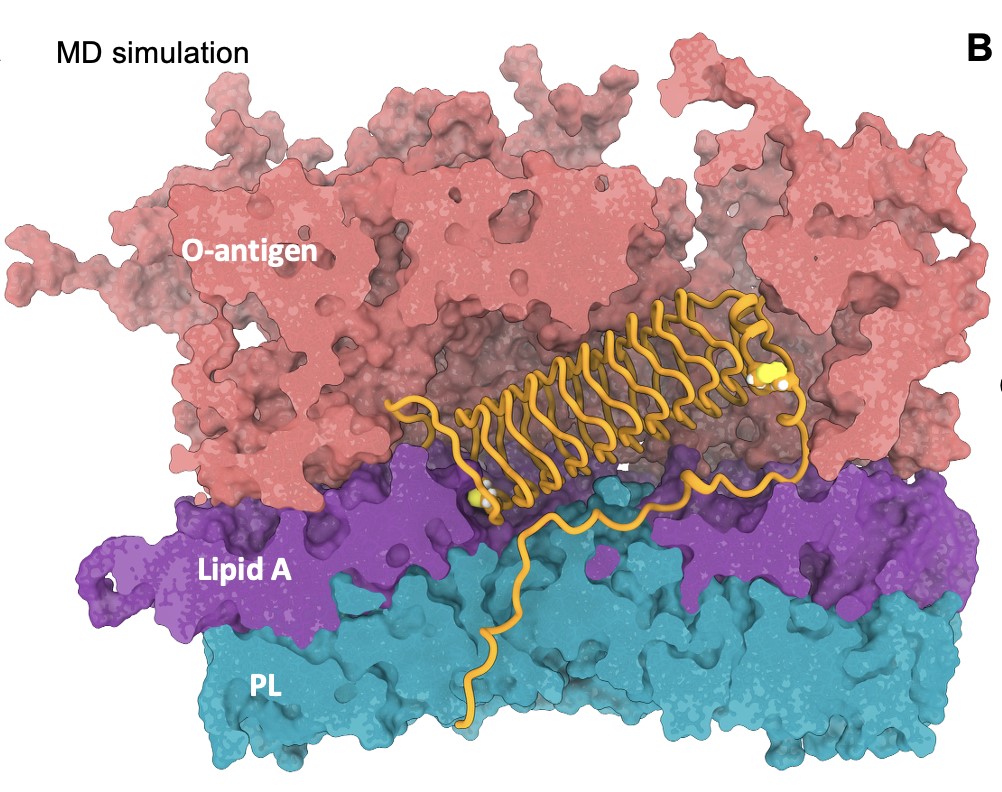
The impermeability of Gram-negative bacteria to large antibiotics is partly due to their outer membrane, an asymmetric layer that acts as an entry barrier. This study discovered a conserved surface protein called YjbI that helps bacteria sense envelope stress and adjust that barrier. When YjbI is lost, bacteria become surprisingly sensitive to two opposite types of antibiotics: small drugs that stimulate drug-efflux pumps, but also large antibiotics that normally cannot traverse the outer membrane. The researchers discovered that loss of YjbI triggers a previously unknown nutrient importer in the outer membrane, called BugA, that serves as entry portal for the two large antibiotics bacitracin and vancomycin. As Zinc stress temporarily removes YjbI, the consequence of this stress is that BugA will be transiently induced and bacteria will become susceptible to bacitracin or vancomycin in this state because they will internalize these antibiotic molecules through BugA.
Understanding how bacteria switch between resistance and sensitivity helps identify new ways to make antibiotics more effective and may guide strategies to overcome antibiotic resistance in harmful bacteria, for example via stress activated nutrient-transporters. This work reveals the dynamically balance antibiotic resistance and vulnerability with nutrient uptake, offering new ideas for antibiotic design. It also prompts future studies aimed at understanding how other nutrient-transporters are regulated that could serve as alternative entry-portals in multidrug-resistant Gram-negative pathogens.
https://link.springer.com/article/10.1038/s44318-025-00668-x