Skeletal Muscle Disorders
Conditions altering skeletal muscle function and mobility
Neuromotor disorders
Numerous conditions impact skeletal muscle functioning, with important deleterious effects on the entire organism and dramatic consequences for the individuals and their caregivers. About 15% of the world's population lives with disability, constituting a major public health challenge. Children and adults with neuromotor disorders (e.g., cerebral palsy, genetic and acquired neuromuscular diseases, stroke) have deficits that directly impact the central command of the movement, the motoneurons and/or the muscles. Of note, neuromuscular diseases, such as amyotrophic lateral sclerosis, muscular dystrophies, and multiple sclerosis, represent a large family of generally rare, acquired and genetic disorders, affecting several hundred thousand patients in Europe alone. Neuromotor disorders lead to muscle weakness and/or muscle atrophy, which impair mobility and ultimately limit the autonomy of the patients, their daily activities and social participation, as outlined by the WHO's International Classification of Functioning, Disability and Health.

@istock
Muscle dysfunction may even threaten their life. Childhood is a critical period for motor skill development and acquisition, and often reveals motor impairment in children with neuromotor disorders. In this context, intervening in the first years of life appears to be more effective than strategies applied later. In line with this, recent innovative therapies targeting early period of neuromotor development, such as intensive goal-directed rehabilitation programs for cerebral palsy or gene therapy for spinal muscular atrophy, aim to reduce motor dysfunction and its broader impact, aligning with the WHO’s REHABILITATION 2030 initiative.
Chronic conditions and Aging
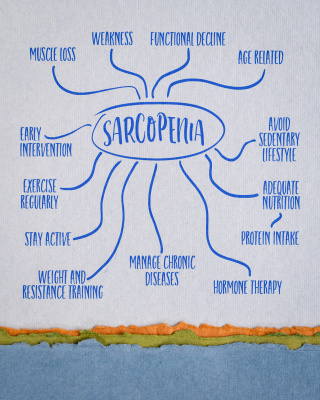
Muscle wasting, along with the subsequent loss of muscle strength, is also a central symptom associated with aging (sarcopenia), which significantly increases frailty, disability and the risk of morbidity and mortality of individuals. Sarcopenia has become a major global public health concern, with projections estimating that 200 million people will be affected by 2058. This condition carries substantial clinical, social, and economic implications, with costs exceeding $20 billion annually in the US alone. Additionally, skeletal muscles are severely affected by prolonged immobilization, such as in intensive care units, and are compromised in conditions, like cancer, AIDS or chronic diseases of the heart, lung or kidney. In these cases, muscle loss can be a critical factor in determining patient survival. Preserving as much muscle strength and function as possible is therefore critical for improving patients’ quality of life and chances of survival. Finally, musculoskeletal disorders, including bone and joint conditions, such as fractures, osteoarthritis or tendon tears, can as well impact skeletal muscle function. These conditions are among the leading causes of disability worldwide, affecting approximately 1.7 billion people. Pain, stiffness, and structural damage in bones and joints often result in altered movement patterns, which can overload or weaken certain muscle groups, reduce physical activity, and contribute to muscle wasting and weakness.
@istock
Sedentarity
In recent years, sedentary behavior has become a widespread lifestyle due to technological advancements and evolving work environments. This shift has significant negative impacts on health, leading to a reduced muscle strength and mass, and increasing the risk of obesity, cardiovascular diseases, type 2 diabetes, and mental health issues. Consequently, physical inactivity not only harms individuals and their families but also imposes a social and economic burden on society. In contrast, regular physical activity offers significant health benefits and serves both as a preventive and therapeutic measure for non-communicable diseases. Scientific evidence robustly supports that physical activity enhances mental health, quality of life, and overall well-being. Health organizations, including the World Health Organization (WHO) and the American Heart Association, recommend at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week.
Overall, regular physical activity, resistance training and personalized therapies are key strategies to preserve muscle function and mitigate the adverse effects of inactivity, aging, chronic diseases, immobilization, as well as numerous neuromuscular and musculoskeletal conditions.
Challenges of translational research on muscular disorders
Working on rare neuromuscular disorders
Translational research aims at understanding the pathomechanisms leading to muscle dysfunction in conditions like neuromotor disorders, musculoskeletal conditions, sarcopenia or malnutrition. Deciphering the pathomechanisms underlying neuromuscular diseases is crucial to design efficient targeted therapies. Moreover, the study of these pathomechanisms can provide insights into fundamental muscle physiology (e.g., on the intricate interplay between neural signaling and muscle function) and broader pathological conditions. More than 90% of genetic neuromuscular diseases are rare disorders (less than 1 person / 100’000). Because of their diversity and rarity, very few research studies are devoted to understanding these conditions. When it comes to therapeutic strategies and clinical trials, neuromuscular diseases are not the priority of pharmacological industries either. Consequently, the molecular mechanisms underlying the onset, the progression and/or the aggravation of muscle dysfunction in these conditions, as well as the development of potent therapeutic strategies remain scarce. Moreover, the rarity of these diseases strongly limits access to patient-derived tissues and cells, and the possibility to drive large-scales studies required to conclude on mechanisms and strategy efficiency. For most of these diseases, diagnosis is delayed because of the rarity, complexity and variability of the symptoms. Some patients suffering from orphan diseases can still even lack a name for their condition, which further contributes to their medical and social isolation and insufficient access to specialized care. In these contexts, the identification of biomarkers for early diagnosis and monitoring, the development of new models and methods to understand the pathologies and assess the efficiency of therapeutic strategies, as well as enhanced international collaborations between research groups and clinicians, are crucial.
Working on sarcopenia
In the last decade, key processes and signaling pathways involved in the onset of sarcopenia (characterized by a reduction in muscle mass and function) have been identified. However, our understanding of this complex condition remains partial, hindering effective management and treatment. Despite recent efforts to reach a consensus regarding the diagnostic criteria to apply, there are still major inconsistencies across clinical institutes. Moreover, recent studies have highlighted the role of impaired proteostasis, denervation, disuse, hormonal changes or inflammation in the progressive loss of muscle mass and force occurring upon aging. To which extent and with which timing these different factors contribute to the onset of sarcopenia is not understood. The genetic and environmental factors influencing individual susceptibility to sarcopenia also remain to be investigated. The development of effective treatments requires proper integration of pathological factors involved in sarcopenia. Development or improvement of methods to adequately evaluate changes in muscle function with age and/or upon treatment is also needed. The lack of a complete picture of the molecular pathomechanisms underlying sarcopenia currently hampers the design of effective interventions and the evaluation of their long-term benefits.
@istock
Working on musculoskeletal disorders
musculoskeletal disorders, although relatively common, remain under-researched regarding their impact on skeletal muscle. Musculoskeletal conditions such as osteoarthritis or tendon tears often involve adaptations in motor control and movement patterns to compensate for pain or lost function. These compensatory adaptations rely on the muscular redundancy of the human body and alternative movement strategies and can mitigate short-term disability. However, it may contribute to long-term dysfunction, such as chronic pain, altered biomechanics, or muscle imbalances, which further degrade physical performance. Translational research in this area is critical to better understand these compensatory mechanisms and their effects on both the progression of musculoskeletal disorders and overall musculoskeletal health.
